For a couple of years now, the World Health Organization has been warning that fake and substandard medicines are on the rise globally. Until recently, the problem has been concentrated largely in countries where most people pay cash for medicines, and where medicine regulation is weak or non-existent. But the hyper-globalised pharmaceutical market is changing that. And the Coronavirus pandemic, an equal-opportunity screwer-up of business-as-usual, is about to bring poor quality medicines to your medicine cabinet, wherever in the world you live.
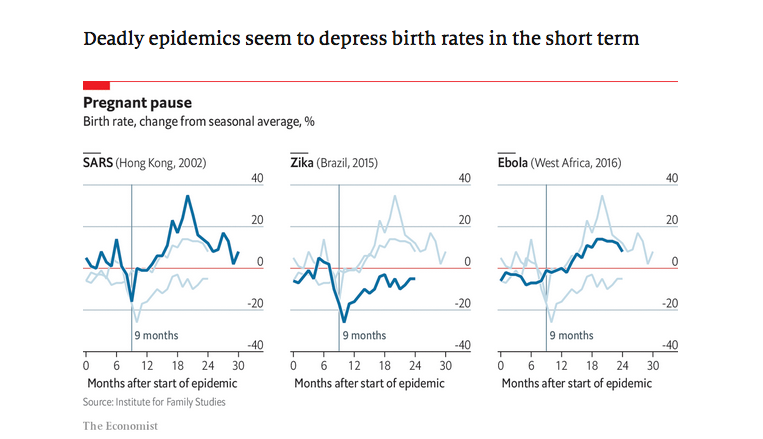
Not just COVID-related meds, you understand. Rising demand, falling supply, public panic, knee-jerk nationalism and distracted regulators will increase the risk of getting bad medicines for diabetes, heart disease, depression, rheumatism, cancer and virtually everything else. In virtually every country.
For a couple of years now, I’ve been working with researchers based in universities and data firms in Indonesia, Singapore, and the Netherlands to figure out why legitimate pharma companies make bad (substandard) medicines, and why people buy and take them. We look at fakes, too. How do the criminals that make them choose what to imitate, and who to sell to? What we’ve learned allows us to predict how Coronavirus will affect medicine quality globally.
It’s no great surprise that the answer to most of the questions above boil down to money, though political pressures have a role to play, too. The details in academic format here (or in this short video). To summarise:
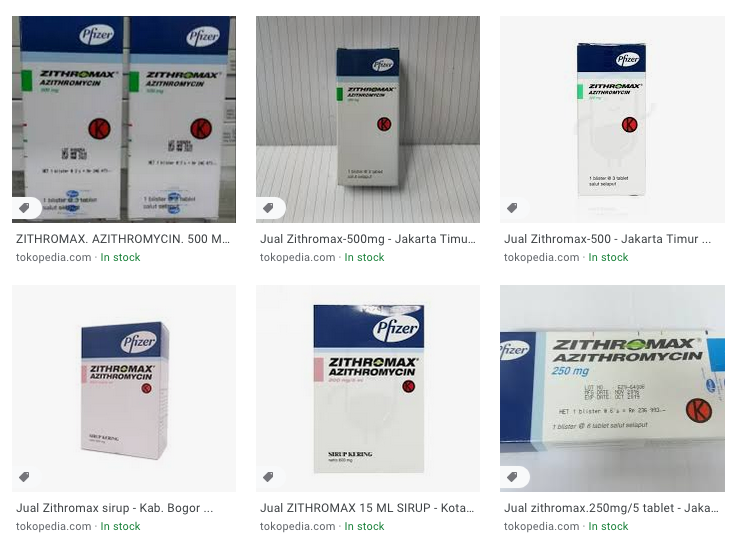
Criminals thinking about making falsified medicines are looking for opportunities to make profits, while minimising their risk of getting caught and punished. Market opportunities are richest when there’s a local shortage of a legit product that people desperately want.
The likelihood of getting away with selling fakes is greatest when:
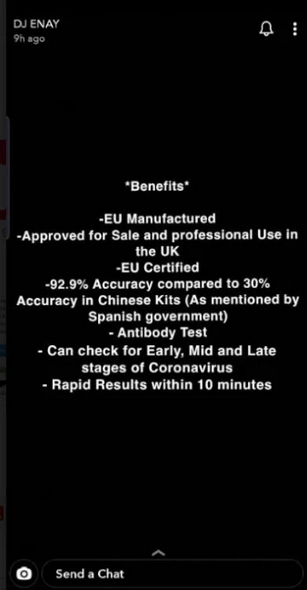
- buyers (at any point in the supply chain) deviate from tried, trusted and effectively regulated sources, or worse, buy online.
- the regulator in the country of sale doesn’t look too closely at medicines once they are already out in the market
- the judicial system is not good at prosecuting or jailing offenders.
Legitimate pharma companies (from big-name multinationals to small generics producers in poorer countries) are also in the business to make money. Squeezed profit margins encourage legitimate manufacturers to cut costs, compromising quality and leading to substandard production.
These substandard meds are most likely to reach patients if:
- the regulator in the country where they are made doesn’t do a good job of overseeing production (sometimes because politicians care more about promoting industry than they do about assuring quality, especially of medicines that will go to patients in other countries);
- the regulator in the country where they are consumed doesn’t do a good job of checking product quality (sometimes because politicians care more about being seen to provide affordable medicines than they do about ensuring that the medicines actually work).
Most better-off countries are subject to some of these factors, but rarely all of them at once. COVID-19 is changing that. We believe the pandemic is going to put all these risk factors on steroids, for lots of products, in lots of markets. Here’s how it will happen:
Falsified medicines
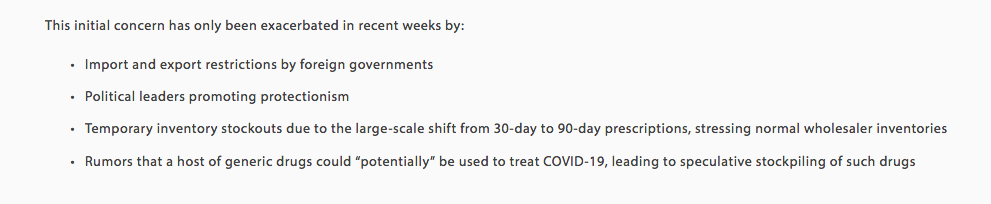
Shortages will create new market opportunities because…
Demand will rise…
1. Demand for products needed for critical care, or that have actual or rumoured therapeutic effects against COVID-19 will rise rapidly in all areas (indeed, it already is!). For critical care products and (hopefully soon-to-be-)proven prophylactics/therapies, this demand will come from institutional buyers (including global health and national procurement agencies) as well as retailers and patients. For products rumoured to be effective, demand will rise more rapidly in the retail sector.
2. Both institutions (possibly including national medical stores) and individuals will buy and stockpile medicines not related to COVID-19. Medicines for life-threatening, chronic conditions, including HIV, diabetes and cardiovascular diseases are especially likely to be affected.
… while supply will fall (at least for some markets)
3. Wherever your medicines are made, the chances are they contain at least some ingredients that come from China, or a very small handful of other countries. For a few active ingredients, there’s only one producer, supplying every manufacturer of finished product worldwide. The supply of active ingredients is threatened by the pandemic (and the quality may be, too.) China’s Zhejiang province, the world’s largest producer of active ingredients, was second worst hit by COVID-19. The impact of COVID-19 related disruption was likely delayed because stocks are routinely built up before the Chinese New Year holiday, when the shut-down began. Northern Italy, another major centre of active ingredient production, has also been very badly hit.
4. China and other exporters of active ingredients will restrict exports to meet their own national needs, further restricting supply to manufacturers in other countries. These restrictions may be applied selectively for political reasons. The US is particularly vulnerable because of the ongoing trade dispute with China; the products that are in highest demand domestically in China, India and other active ingredient-producing countries will be worst hit.
5. Countries that manufacture finished medicines will also restrict exports of medicines in order to meet national demand. India, which is the world’s largest exporter of finished medicines, has already started restricting exports. That’s in part because India, which imports around two thirds of its active ingredients, is having a hard time getting the raw materials it needs. Last year, about 70% of its raw pharma imports came from China, and a further 11% from Italy. Export restrictions from India and other low-cost manufacturers will have a huge knock-on effect in the US, Europe and elsewhere.
6. Countries and large institutions will rebuild stockpiles, and profiteering distributors might hold on to medicines too, trying to drive the price up. This will cause localised shortages. In some countries, where public budgets are especially strained, medicines may be drained out of the public health systems to fatten the cushion under the private sector.
7. Manufacturers may face political pressure to switch production capacity to COVID-19-related medicines, disrupting the supply of other essential medicines. We’ve already seen car companies pressed into service to produce ventilators, but that’s fine, we can still drive last year’s car. When a maker of cancer drugs switches to making antivirals, the cancer patient dies.
8. A system-wide focus on COVID-19 coupled with disruptions to normal workflows will derail routine public procurement systems in some countries, leading to auction failures and shortages in the public sector.
9. Supply restrictions will push prices up. Countries with limited budgets for health may cut the number of medicines they buy, leaving patients to pick up the tab. Faced with buying more, higher-priced medicines, families may choose to “go cheap” — to buy medicines on the internet or from less reputable sources, contributing to risk 14, below.
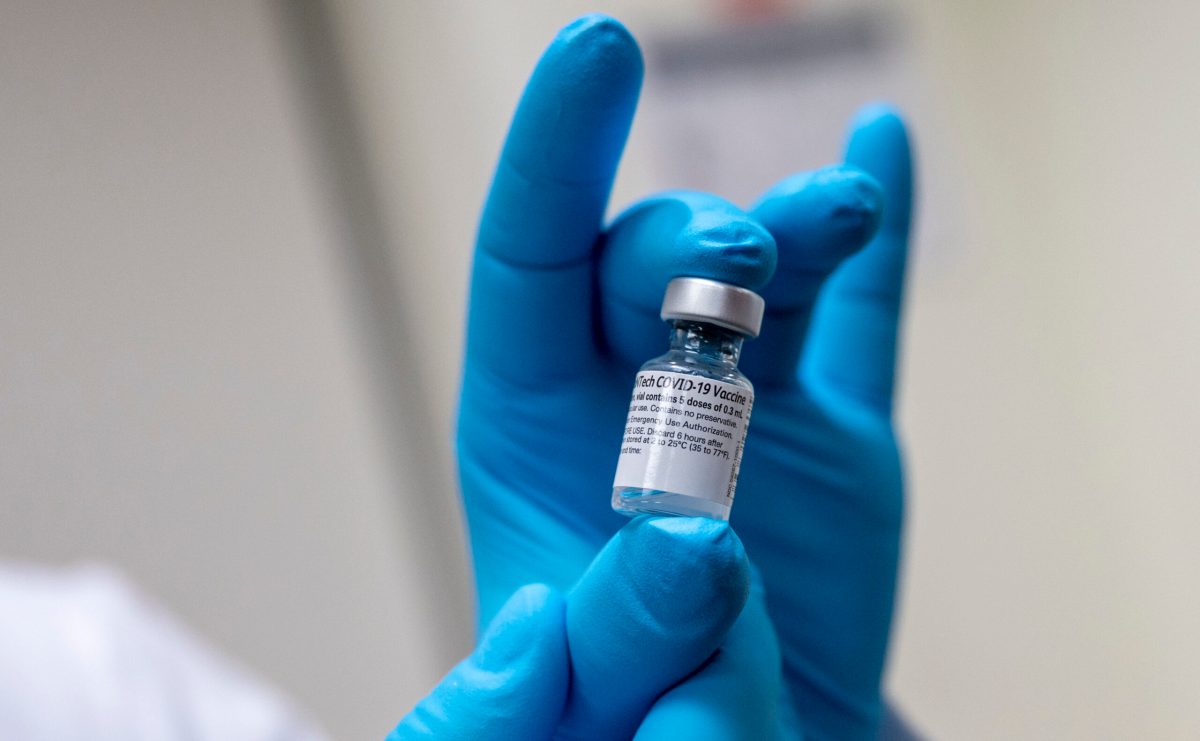
10. Restricted transport, especially air traffic, will push up the cost of distribution, and reduce the timely delivery of medicines, creating localised shortages. Products such as vaccines, which need to be kept cold and transported quickly, will be especially at risk.
Meanwhile, profits for falsifiers will rise
11. The cost of making a fake pill is more or less the same, whatever you’re pretending is in it. Falsifiers usually target higher-end meds, because they make more money per pill, for roughly the same amount of risk (though they avoid hospital-only products, as well as those they know are most effectively policed by manufacturers). As shortages push prices up, the profit margin for falsifiers will rise on lower-priced medicines, encouraging more falsification of high-volume items that people are desperate to get hold of. These include medicines for high-prevalence chronic conditions, including diabetes and cardiovascular diseases, and in some markets HIV, TB and malaria medicines.
Risk of getting caught will fall because…
More buyers will step out of regulated and/or secure supply chains…
12. Shortages (1–10), disruptions to public procurement (8), and strong political pressure to be seen to be providing medicines will oblige more institutional buyers to source medicines from previously untested suppliers. This increases opportunities for falsifiers to introduce products to the supply chain.
13. When products are in short supply, it’s a seller’s market. Quality-assured distributors are going to serve their best clients first, and to them, their best clients are the ones that pay top dollar, on time. In lots of countries, national health systems are strapped for cash as well as strapped up in red tape, and are particularly bad at paying bills on time. They’re going to be dumped by their regular suppliers, and may have to look elsewhere for stocks.
14. With people stuck at home, or going to the health centre or pharmacy and facing empty shelves or sticker-shockingly high prices, sales of medicines on the internet will increase. The internet is an open door for falsifiers.
… and regulatory oversight over supply chains will be eroded
15. As governments concentrate human and financial resources on limiting the spread and impact of the pandemic, regulatory attention and laboratory capacity will be diverted. Together with restrictions on movement, this will disrupt oversight of supply chains, and reduce the already infinitesimally small proportion of products whose quality gets checked on import, or once it’s in the supply chain.
Substandard medicines
Profit margins will be increasingly squeezed because…
Production and distribution costs will rise
16. As we said earlier, the cost of raw materials will rise. They will be pushed up further for importing nations by restrictions on transport, and in some cases by falls in the local currency.
17. Increased illness, absenteeism or death in the workforce will push up costs to producers and distributors, especially in countries hardest hit by COVID-19.
18. Restricted transport, especially air traffic, pushes up the cost of distribution. (There’s also a direct effect on quality, because medicines, especially those which are more volatile, can degrade if they sit around in shipping containers or in poorly-cooled warehouses.
…while income may fall
19. Shortages of active ingredients will reduce production volumes for some producers; this may not be offset by rising prices for finished product. Producers that are locked in to longer-term contracts with large buyers will suffer most.
20. Recession, diversion of health spending to COVID-19-related products, or a general squeeze on public finances may reduce public funding available for other medicines.
21. Export restrictions may restrict sales to clients in higher-paying markets.
22. Political pressure to produce COVID-19 related products for public procurement may divert production from more lucrative products. This will especially be a problem in countries with large, state-affiliated medicine producers.
23. Sale of some relatively lucrative over-the-counter products may be reduced as a result of restrictions on movement, or simply because people don’t have spare cash to buy any medicines that they think are not a matter of life or death.
The squeeze on margins will lead to strong pressure on producers to cut costs where possible. The relatively high and rising price of active ingredients, coupled with shortages, suggest that reductions in the quality and quantity of active ingredient may be a common cost-cutting response.
Technical capacity won’t always be up to scratch
24. In many countries, the pandemic has sparked a lot of political grandstanding about national resilience and self-reliance, and this is in some places being translated into a push for rapid development or scale-up of local pharmaceutical production, even when the expertise, machinery or ingredients available locally are inadequate. That’s a good recipe for substandard medicines (we’re already seeing it in protective equipment).
25. Rapid scale-up of newly-developed COVID-19-specific vaccines or therapies may be especially vulnerable to production errors in the early stages, simply because there’s not much experience making them yet, especially on a large scale. We’ve seen this recently, in the case of substandard test kits shipped from China to Spain.
But errors are less likely to be spotted by regulators
26. The COVID-19 response is likely to disrupt routine regulatory functions. While the spotlight is on medicines and equipment needed to respond to the pandemic, regular inspections of factories and distribution chains for other, more common medicines may be winnowed down. So if any of the factors above are eating into quality, the problem is less likely to be spotted.
27. Political pressure to ramp up domestic production, as well as public pressure to deliver new medicines, may oblige regulators to fast-track products, or discourage them from being too strict on companies that are being called on to help out in a crisis.
What can we do about it?
Most of these problems are rooted in two fundamental (and intertwined) mismatches in the global economy. First, we increasingly look to governments to ensure that demand for affordable medicines is met, while relying on profit-seeking companies to supply that demand. That leads to procurement and production practices that incentivise cost-cutting and undermine product quality.
Second, we want both the price-lowering (and pollution-outsourcing) efficiencies of a globalised supply chain, while simultaneously demanding security of supply at the national level. As the current pandemic is teaching us, you can’t have it both ways.
Fixing those fundamental flaws in the global economic model is way above the pay grade of our research team. But in the meantime, we can use our analysis at least to flag up which medicines are most at risk, right now. None of the factors above is, all by itself, a clear indicator that a particular medicine is overly likely to be substandard or falsified. But when factors 1–15 are combined into an index:
Indicators of rising demand and indicators of restricted supply and indicators of good potential profits and indicators of low risk of getting caught; for a specific product (and sometimes even a specific brand) in a specific market…
… then we have a clear indication that the product might well be a fake. Regulators can use the index as an early warning system to trigger inspections, and to warn pharmacists and the public to view particular products or sources of supply with caution.
Ditto for factors 16–27; if a product ticks a lot of those boxes simultaneously, it’s at high risk of being substandard. If the national regulator is unable to respond by ramping up inspections and closing non-compliant producers, either because they are politically hamstrung or because they don’t have the capacity, a flagging system can at least help buyers to make better choices.
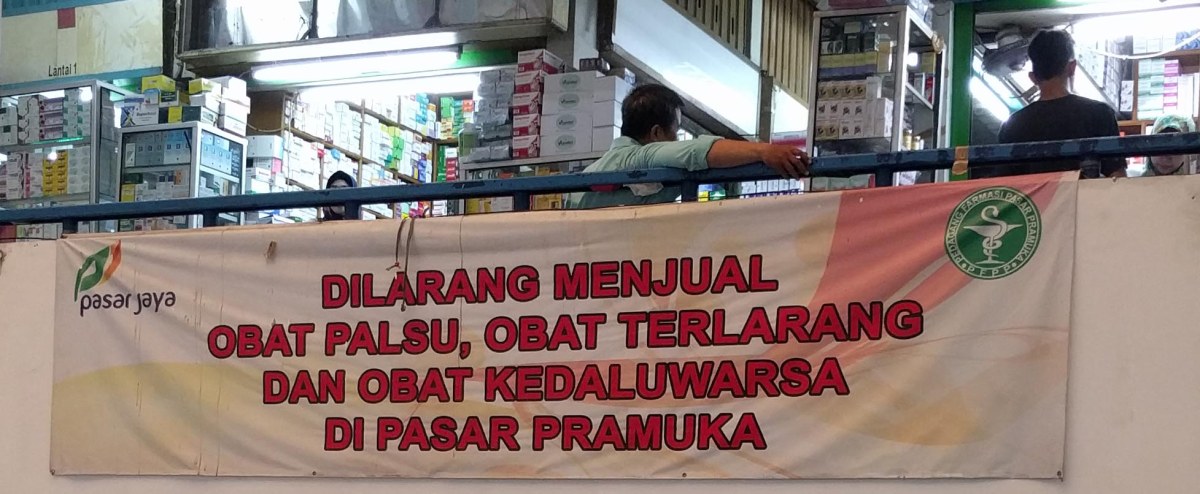
In Indonesia, where some of us are based, we were (before the pandemic struck) working with the national medicine regulator to try out a system that uses market data to flag products at high risk of being substandard or falsified (we call it MedsWatch). We’re still in the early stages, but it looks like it works pretty well. Well enough, indeed, to justify retooling our indicators for the 27 risk factors listed above, to develop an early warning system for the quality of medicines affected by the COVID-19 pandemic.
Watch this space. And in the meantime, please don’t stockpile meds (which will contribute to lots of problems for other people), or buy your pills from unregulated online stores (which may well end up being a problem for you yourself)
Thanks to Steven Harsono
Written by Elizabeth Pisani